In the world of emergency medical services (EMS), few situations are as time-sensitive as cardiac arrest. Every second counts when it comes to the survival and recovery of individuals experiencing a cardiac event. Quick response times by EMTs and paramedics can mean the difference between life and death, as immediate medical intervention dramatically improves the chances of survival and long-term outcomes. In densely populated areas like Los Angeles and Southern California, ensuring fast and effective response to cardiac arrest cases is a priority for EMS providers like LifeLine EMS.
This article explores why rapid response times are critical in cardiac arrest cases, the factors that influence these response times, and how LifeLine EMS is committed to delivering fast, life-saving care when it matters most.
What Happens During Cardiac Arrest?
Cardiac arrest occurs when the heart suddenly stops beating, preventing blood from being pumped to the brain and other vital organs. Unlike a heart attack, which is caused by a blockage in the arteries, cardiac arrest is often triggered by an electrical disturbance in the heart. This condition causes the heart to stop functioning properly, leading to a complete cessation of blood flow throughout the body.
Key Symptoms of Cardiac Arrest:
- Sudden collapse: The person may suddenly lose consciousness.
- No pulse: There is no detectable heartbeat.
- No breathing: The individual is not breathing or is gasping for air.
- Unresponsiveness: The person does not respond to external stimuli.
Without immediate intervention, cardiac arrest is almost always fatal. Every minute that passes without treatment decreases the victim’s chances of survival by 7% to 10%. After 10 minutes without medical intervention, the likelihood of resuscitation drops significantly, and even if the patient is revived, the risk of severe brain damage increases.
Why Quick Response Time is Crucial
Quick response time in cardiac arrest cases is essential because it directly affects patient survival and recovery. The goal of EMS professionals is to initiate life-saving interventions as quickly as possible to restore the heart’s normal rhythm and maintain blood flow to the brain and other vital organs.
1. The “Chain of Survival”
The American Heart Association (AHA) outlines a concept known as the “Chain of Survival,” which emphasizes the steps that must be taken during a cardiac arrest to increase the chances of survival. A rapid EMS response is one of the most crucial links in this chain.
- Early Recognition and Activation of EMS: Recognizing cardiac arrest and calling 911 immediately is the first step in the chain of survival.
- Early CPR: Bystander-administered CPR can help maintain blood flow until EMS arrives. CPR is most effective when started within the first few minutes after cardiac arrest.
- Rapid Defibrillation: Defibrillation is the process of delivering an electric shock to the heart to restore a normal rhythm. EMS responders are equipped with defibrillators, and the sooner a defibrillator is used, the higher the chance of survival.
- Advanced Life Support and Post-Resuscitation Care: Once on the scene, EMTs and paramedics can provide advanced life support, including airway management, medication, and continued defibrillation if necessary.
The effectiveness of each step in the chain of survival hinges on the speed at which EMS responders arrive and begin treatment.
2. Reducing Brain Damage
One of the most critical factors in cardiac arrest cases is the amount of time the brain is deprived of oxygen. Without adequate blood flow, brain cells begin to die within minutes. Irreversible brain damage can occur within 4 to 6 minutes of cardiac arrest. This makes it vital for EMS teams to arrive on the scene quickly and begin interventions such as CPR, defibrillation, and ventilation.
- CPR to Maintain Blood Flow: EMTs and paramedics are trained to perform high-quality CPR, which can temporarily maintain blood flow to the brain and heart until more advanced treatment is available.
- Defibrillation to Restore Heart Rhythm: If defibrillation is performed within the first few minutes of cardiac arrest, the chances of restoring a normal heart rhythm are significantly higher, which can help prevent brain damage.
3. Improving Long-Term Outcomes
Rapid response times don’t just increase the likelihood of survival—they also improve long-term outcomes for cardiac arrest patients. The quicker the EMS team can restore the heart’s rhythm and blood flow, the better the chances of minimizing damage to the heart and brain.
- Higher Survival Rates: Studies have shown that response times of less than 8 minutes are associated with higher survival rates for cardiac arrest patients.
- Reduced Risk of Neurological Damage: Fast EMS intervention reduces the risk of permanent neurological damage, enabling patients to recover with better cognitive and motor function after resuscitation.
Factors Affecting Response Time
Several factors can influence how quickly EMS providers are able to respond to a cardiac arrest emergency. These factors vary based on location, traffic conditions, and resource availability.
1. Geographic Location
Response times can vary significantly depending on the geographic location of the emergency. In rural or remote areas, EMS units may take longer to reach a patient due to longer travel distances. In urban areas like Los Angeles, the density of traffic and the layout of the streets can affect how quickly an ambulance can reach the scene.
2. Traffic Conditions
Traffic congestion is a common challenge in metropolitan areas like Los Angeles, where heavy traffic can delay EMS response times. To mitigate this, EMS providers such as LifeLine EMS utilize advanced dispatch systems with GPS technology to identify the quickest and most efficient routes to the emergency.
- GPS-Enabled Dispatch: GPS technology helps dispatchers direct ambulances to the scene via the fastest routes, reducing delays caused by traffic or road closures.
- Strategic Ambulance Deployment: EMS providers in busy areas often use strategic ambulance placement, positioning units in high-demand locations to ensure faster response times during peak hours.
3. Availability of Resources
The availability of EMS units is another factor that impacts response times. In areas with a high volume of emergency calls, ambulances may be tied up responding to other incidents, potentially delaying response to new emergencies. LifeLine EMS works to ensure that its fleet of ambulances is adequately staffed and distributed to handle high volumes of calls efficiently.
4. Public Awareness and Bystander Action
In cardiac arrest cases, public awareness and bystander action also play a role in improving outcomes. Prompt recognition of the signs of cardiac arrest and the immediate initiation of CPR by a bystander can significantly improve the chances of survival while waiting for EMS to arrive.
- CPR Training: By educating the public about the importance of CPR and how to perform it, EMS providers can empower individuals to take life-saving actions before professional help arrives.
How LifeLine EMS Ensures Quick Response Times in Cardiac Arrest Cases
LifeLine EMS understands the importance of rapid response in cardiac arrest cases and has implemented several strategies to ensure that its EMTs and paramedics can respond quickly and effectively.
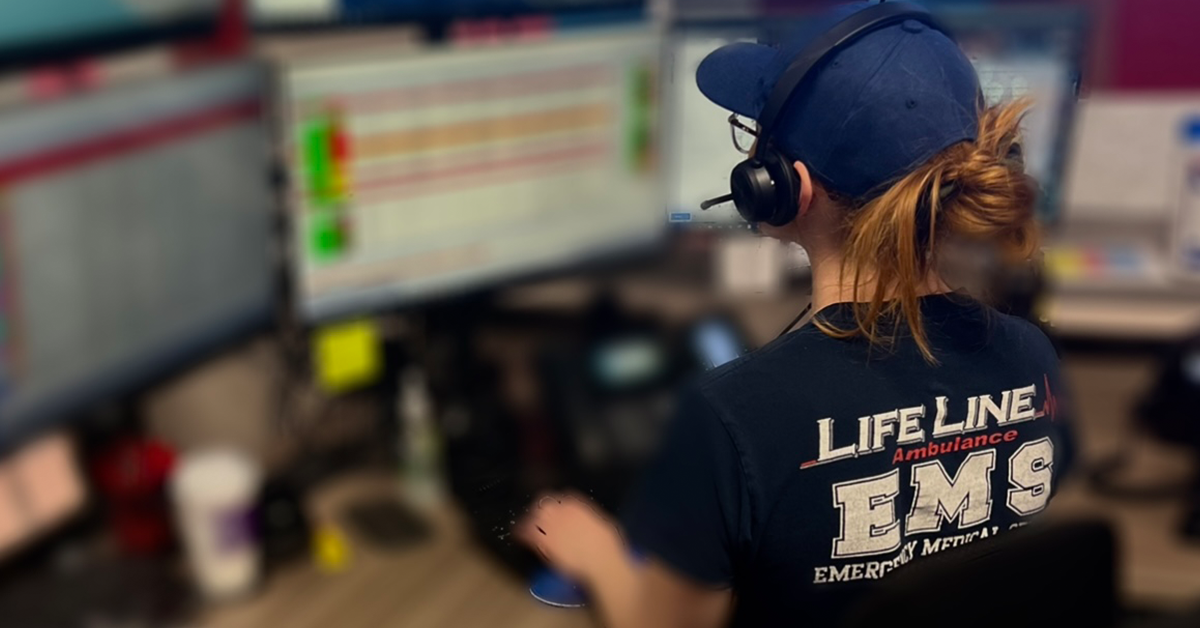
1. Advanced Dispatch Technology
LifeLine EMS uses cutting-edge dispatch technology that integrates GPS, real-time traffic data, and predictive analytics to optimize ambulance routes and reduce response times. This allows EMS teams to reach the scene of a cardiac arrest as quickly as possible, even in congested areas of Los Angeles and Southern California.
- Real-Time Traffic Monitoring: Dispatchers at LifeLine EMS monitor traffic conditions in real-time, ensuring that ambulances are dispatched via the fastest routes to avoid delays.
- Optimized Ambulance Placement: By analyzing historical data on call volume and location, LifeLine EMS strategically positions ambulances in areas where cardiac arrest incidents are most likely to occur, improving response times.
2. Ongoing Training for EMTs and Paramedics
To ensure that EMTs and paramedics are always prepared to respond to cardiac arrest cases, LifeLine EMS provides continuous training on CPR, defibrillation, and advanced cardiac life support (ACLS) protocols. This training ensures that EMS personnel can quickly assess a patient’s condition and administer the appropriate interventions upon arrival.
- High-Quality CPR Training: EMTs and paramedics at LifeLine EMS are trained to perform high-quality chest compressions, which are critical for maintaining blood flow in cardiac arrest patients.
- Defibrillator Proficiency: EMS personnel are proficient in using automated external defibrillators (AEDs) and manual defibrillators, allowing them to deliver timely shocks to restore a patient’s heart rhythm.
3. Collaboration with Hospitals
LifeLine EMS collaborates closely with local hospitals to ensure that patients receive timely and appropriate post-resuscitation care. Communication between EMS teams and hospital staff begins before the patient arrives, enabling hospitals to prepare for advanced cardiac care and improve the chances of a successful outcome.
- Pre-Hospital Communication: EMTs and paramedics provide detailed information about the patient’s condition and the interventions administered en route, allowing hospital teams to be fully prepared for the patient’s arrival.
Keep Reading
Want more? Here are some other blog posts you might be interested in.
In the high-stakes world of emergency medical services, clear and effective communication can mean the difference between life and death. EMS professionals...
Emergency Medical Services is an ever-evolving field that requires constant learning and adaptation. With medical advancements, technological innovations, and increasing public health...
Emergency Medical Services s a high-stress, physically demanding profession that requires dedication, quick decision-making, and resilience. While the rewards of saving lives...