Mental health emergencies are becoming increasingly prevalent in communities across the United States, including Los Angeles and Southern California. From anxiety crises to severe psychiatric episodes, these emergencies require a unique approach that prioritizes compassion, de-escalation, and connection to appropriate care. Emergency Medical Services (EMS) providers are on the frontlines of responding to mental health crises, often serving as the first point of contact for individuals in distress.
The Growing Need for EMS Support in Mental Health Emergencies
The demand for mental health emergency services is increasing as more people face mental health challenges. Factors such as societal stress, economic instability, and the lingering effects of the pandemic have contributed to a rise in mental health crises. For EMS providers, this means responding to a wider variety of emergencies that involve behavioral health needs.
Key Statistics on Mental Health Emergencies:
- Increased 911 Calls: Studies show that up to 20% of 911 calls involve a mental health crisis.
- Limited Resources: In many areas, mental health facilities and crisis intervention services are overburdened, leaving EMS providers to fill the gap in immediate care.
- Dual Diagnosis Cases: Many individuals in crisis also struggle with substance use disorders, complicating the response and requiring specialized care.
The Role of EMS Providers in Mental Health Emergencies
EMS providers are uniquely positioned to respond to mental health emergencies because they are trained to assess situations quickly, manage immediate safety concerns, and connect individuals to appropriate resources. Their role extends beyond medical care to include emotional support and crisis de-escalation.
Key Responsibilities of EMS Providers in Mental Health Crises:
- Assessing the Situation:
- EMS personnel evaluate the severity of the crisis, taking into account both medical and psychological factors.
- This includes identifying any immediate safety threats to the individual, EMS personnel, or others at the scene.
- De-escalation:
- A calm, empathetic approach is essential for de-escalating situations involving individuals in distress.
- EMS teams use verbal and non-verbal communication techniques to reduce tension and establish trust.
- Providing Immediate Care:
- EMS providers address any medical concerns, such as injuries or symptoms caused by self-harm, substance use, or physical agitation.
- Basic life support (BLS) measures may be necessary if the individual’s physical health is at risk.
- Transporting to Appropriate Facilities:
- EMS teams work with local hospitals, psychiatric facilities, and crisis intervention centers to ensure the individual receives specialized care.
- Transport decisions are based on the individual’s condition, the availability of resources, and the severity of the crisis.
Specialized Training for Mental Health Emergencies
EMS providers receive specialized training to equip them with the skills needed to handle mental health emergencies effectively. This training focuses on understanding mental health conditions, employing de-escalation techniques, and working collaboratively with mental health professionals.
1. Crisis Intervention Training (CIT)
Crisis Intervention Training is a cornerstone of EMS education for mental health emergencies. CIT programs teach EMS personnel how to recognize signs of mental health disorders and respond with compassion and professionalism.
- Understanding Mental Illness: EMS teams learn about common mental health conditions, such as depression, bipolar disorder, schizophrenia, and PTSD, as well as how these conditions can manifest during a crisis.
- Empathy and Communication: CIT emphasizes the importance of active listening, empathy, and non-judgmental communication to build rapport with individuals in crisis.
- Safety and De-escalation: Providers are trained in techniques to safely de-escalate situations, reducing the need for physical restraint or law enforcement involvement.
2. Trauma-Informed Care
Trauma-informed care is an essential component of EMS training for mental health emergencies. This approach recognizes the impact of past trauma on an individual’s behavior and prioritizes creating a sense of safety and trust.
- Avoiding Retraumatization: EMS personnel are trained to avoid actions that may inadvertently exacerbate the individual’s distress, such as loud commands or sudden movements.
- Empowering Individuals: Trauma-informed care focuses on giving individuals a sense of control over their situation, such as involving them in decisions about their care.
3. Collaborative Training with Mental Health Professionals
Many EMS providers partner with mental health experts to offer joint training sessions, which provide insights into best practices for managing complex mental health cases.
- Scenario-Based Training: Role-playing and simulated scenarios help EMS teams practice responding to mental health emergencies in a controlled environment.
- Co-Responder Models: Some EMS systems train personnel to work alongside mental health professionals, such as social workers or crisis counselors, during responses.
Technology and Tools for Managing Mental Health Emergencies
Advancements in technology have enhanced the ability of EMS providers to respond effectively to mental health crises. These tools improve communication, streamline care coordination, and support decision-making.
1. Mobile Crisis Units
Mobile crisis units are specialized EMS teams equipped to respond specifically to mental health emergencies. These units often include mental health professionals who work alongside EMTs and paramedics to provide on-scene assessment and intervention.
2. Telehealth Integration
Telehealth technology allows EMS teams to connect individuals in crisis with remote mental health professionals. This real-time consultation ensures that patients receive expert guidance, even in areas where mental health resources are limited.
- Virtual Assessments: Mental health professionals can assess individuals via video calls, providing recommendations for care and next steps.
- Resource Coordination: Telehealth enables EMS teams to identify available psychiatric beds or connect patients to outpatient services.
3. Electronic Patient Care Reporting (ePCR)
ePCR systems streamline the documentation process, ensuring that critical information about the individual’s condition and EMS interventions is shared with receiving facilities. This improves continuity of care and reduces the risk of miscommunication.
Challenges in Responding to Mental Health Emergencies
While EMS providers play a crucial role in mental health emergencies, they face several challenges in delivering optimal care.
1. Limited Mental Health Resources
Many communities, including those in Southern California, face shortages of mental health facilities and professionals. This can result in delays in accessing care or an overreliance on emergency departments.
2. Stigma Around Mental Health
Stigma remains a barrier to seeking help for mental health issues. EMS teams often encounter individuals who are reluctant to engage with care due to fear of judgment or misunderstanding.
3. Complex Cases
Mental health emergencies often involve co-occurring conditions, such as substance use disorders or physical health issues, making assessment and intervention more complex.
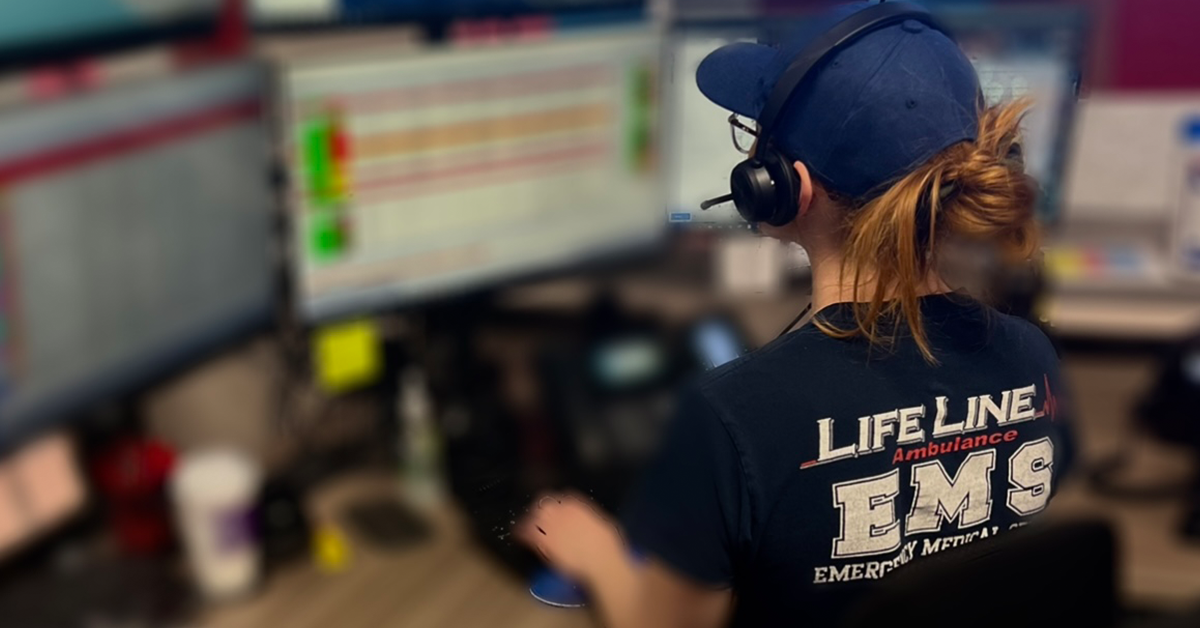
How LifeLine EMS Supports Mental Health Emergencies in Los Angeles
LifeLine EMS is committed to providing compassionate, professional care for individuals experiencing mental health crises. As a leading EMS provider in Los Angeles and Southern California, LifeLine EMS prioritizes the safety, dignity, and well-being of every patient.
1. Highly Trained Teams
LifeLine EMS ensures that its EMTs and paramedics receive specialized training in mental health care, including crisis intervention, de-escalation techniques, and trauma-informed practices. This training equips them to handle a wide range of behavioral health emergencies with professionalism and empathy.
2. Collaborative Partnerships
LifeLine EMS works closely with local hospitals, psychiatric facilities, and community organizations to coordinate care for individuals in crisis. These partnerships ensure that patients are connected to appropriate resources quickly and efficiently.
3. Advanced Technology
By leveraging technology such as telehealth and ePCR systems, LifeLine EMS enhances its ability to provide high-quality care during mental health emergencies. These tools improve communication, streamline documentation, and support seamless transitions of care.
4. Community Education
LifeLine EMS actively engages in community outreach and education initiatives, raising awareness about mental health and reducing stigma. By educating the public about recognizing and responding to mental health crises, LifeLine EMS empowers communities to take proactive steps toward mental well-being.
Keep Reading
Want more? Here are some other blog posts you might be interested in.
In the high-stakes world of emergency medical services, clear and effective communication can mean the difference between life and death. EMS professionals...
Emergency Medical Services is an ever-evolving field that requires constant learning and adaptation. With medical advancements, technological innovations, and increasing public health...
Emergency Medical Services s a high-stress, physically demanding profession that requires dedication, quick decision-making, and resilience. While the rewards of saving lives...