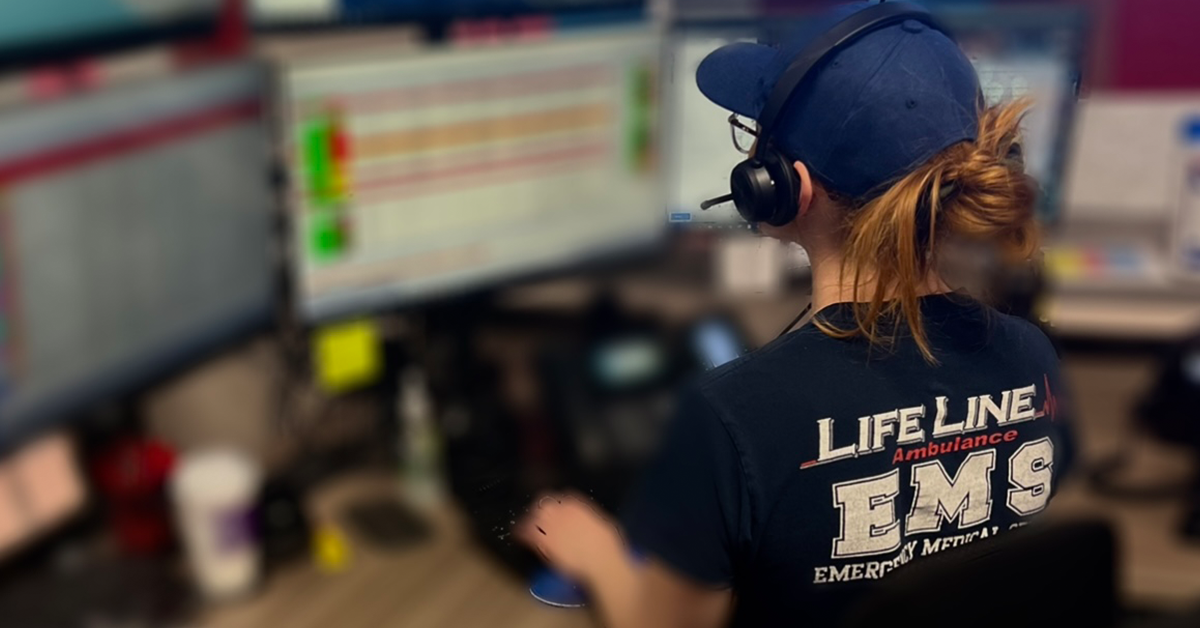
In emergency medical services, a seamless handoff at the emergency room is crucial for patient safety and effective care. The transition from EMS providers to hospital staff must be efficient, accurate, and thorough to ensure continuity of care. LifeLine EMS has developed robust strategies to facilitate smooth patient handoffs, particularly in the fast-paced environments of Los Angeles and Southern California. By leveraging structured communication, advanced technology, and strong hospital partnerships, LifeLine EMS ensures that every patient receives the best possible care upon arrival at the ER.
The Importance of Effective EMS to ER Handoffs
A well-executed EMS handoff can mean the difference between life and death. Proper communication ensures that critical patient information is accurately conveyed to ER teams, allowing for prompt diagnosis and treatment. Ineffective handoffs can lead to delays, medical errors, and decreased patient outcomes. In high-demand areas like Los Angeles, where emergency rooms experience a constant influx of patients, streamlining handoffs is essential.
Key Challenges in EMS to ER Handoffs
Despite its importance, EMS-to-ER handoff processes face several challenges, including:
- Time Constraints: EMS teams must quickly relay vital patient information while balancing the urgency of transporting other patients.
- Communication Gaps: Differences in terminology and documentation between EMS and hospital staff can lead to misunderstandings.
- High-Stress Environment: Emergency rooms are often chaotic, making it difficult to ensure focused, uninterrupted handoffs.
- Variability in Hospital Protocols: Each hospital may have different expectations for incoming patient reports, requiring EMS providers to adapt to multiple systems.
How LifeLine EMS Ensures Seamless Handoffs
1. Standardized Handoff Protocols
LifeLine EMS follows structured communication frameworks to ensure that all essential patient data is conveyed efficiently. The most commonly used tool is the SBAR (Situation, Background, Assessment, Recommendation) protocol, which organizes patient information into:
- Situation: Why the patient was transported.
- Background: Medical history and relevant conditions.
- Assessment: Patient’s vital signs, symptoms, and current condition.
- Recommendation: Suggested next steps for hospital staff.
2. Pre-Arrival Alerts to Emergency Rooms
To expedite patient care, LifeLine EMS uses advanced notification systems to alert hospitals before patient arrival. These alerts provide real-time information on:
- Patient’s medical condition.
- Estimated time of arrival.
- Critical interventions already performed.
- Special needs (e.g., trauma team activation, cardiac unit readiness).
By preparing hospital teams in advance, LifeLine EMS reduces wait times and facilitates smoother transitions upon arrival.
3. Use of Advanced Technology
Technology plays a crucial role in streamlining EMS handoffs. LifeLine EMS incorporates:
- Electronic Patient Care Reports (ePCRs): Digital documentation systems that capture real-time patient data and transfer it to ER teams before arrival.
- Telemetry Systems: Wireless transmission of vital signs to hospital monitors, enabling doctors to assess a patient’s condition in real-time.
- GPS Tracking: Allows ER personnel to anticipate ambulance arrival and prepare necessary resources in advance.
4. Collaboration with Hospitals
LifeLine EMS has established strong partnerships with hospitals across Southern California. Regular meetings and training sessions between EMS providers and ER staff ensure alignment on protocols and expectations. These collaborations help refine processes and address potential inefficiencies in patient transitions.
5. Continuous Training for EMS Personnel
To maintain high standards of patient care, LifeLine EMS emphasizes ongoing training for its paramedics and EMTs. This training includes:
- Simulation-Based Handoff Training: Realistic drills that mimic ER handoff scenarios to reinforce best practices.
- Interdisciplinary Communication Workshops: Training to enhance dialogue between EMS and hospital staff.
- Medical Updates and Protocol Reviews: Keeping EMS teams informed on the latest hospital requirements and emergency care advancements.
6. Specialized Handoff Approaches for High-Risk Patients
Some patients require extra attention during handoffs, such as:
- Cardiac Arrest Patients: LifeLine EMS teams provide detailed CPR reports, medication administered, and response to treatment before hospital arrival.
- Trauma Patients: Quick, concise handoffs that align with trauma team protocols to expedite care.
- Pediatric Patients: Clear communication with pediatric specialists to ensure child-specific interventions are considered immediately.
Future Innovations in EMS Handoffs
LifeLine EMS continues to explore emerging technologies and process improvements, including:
- AI-Driven Predictive Analytics: Using artificial intelligence to assess patient conditions and recommend treatment strategies before ER arrival.
- Wearable Biometric Devices: Providing continuous monitoring and real-time data transfer to hospital teams.
- Augmented Reality (AR) Training Modules: Enhancing EMS training with immersive, interactive learning experiences to refine handoff skills.
Keep Reading
Want more? Here are some other blog posts you might be interested in.
In the high-stakes world of emergency medical services, clear and effective communication can mean the difference between life and death. EMS professionals...
Emergency Medical Services is an ever-evolving field that requires constant learning and adaptation. With medical advancements, technological innovations, and increasing public health...
Emergency Medical Services s a high-stress, physically demanding profession that requires dedication, quick decision-making, and resilience. While the rewards of saving lives...