When someone dials 911 for a medical emergency, the response seems almost instantaneous. However, behind every EMS call is a sophisticated system of protocols, communications, and medical interventions designed to ensure the best possible patient outcome. In a fast-paced metropolitan area like Los Angeles and Southern California, EMS teams must navigate complex logistics, traffic, and medical decisions in real-time.
This article breaks down the entire lifecycle of an EMS call, from the moment an emergency is reported to patient handoff at a medical facility, highlighting the critical steps taken behind the scenes to save lives.
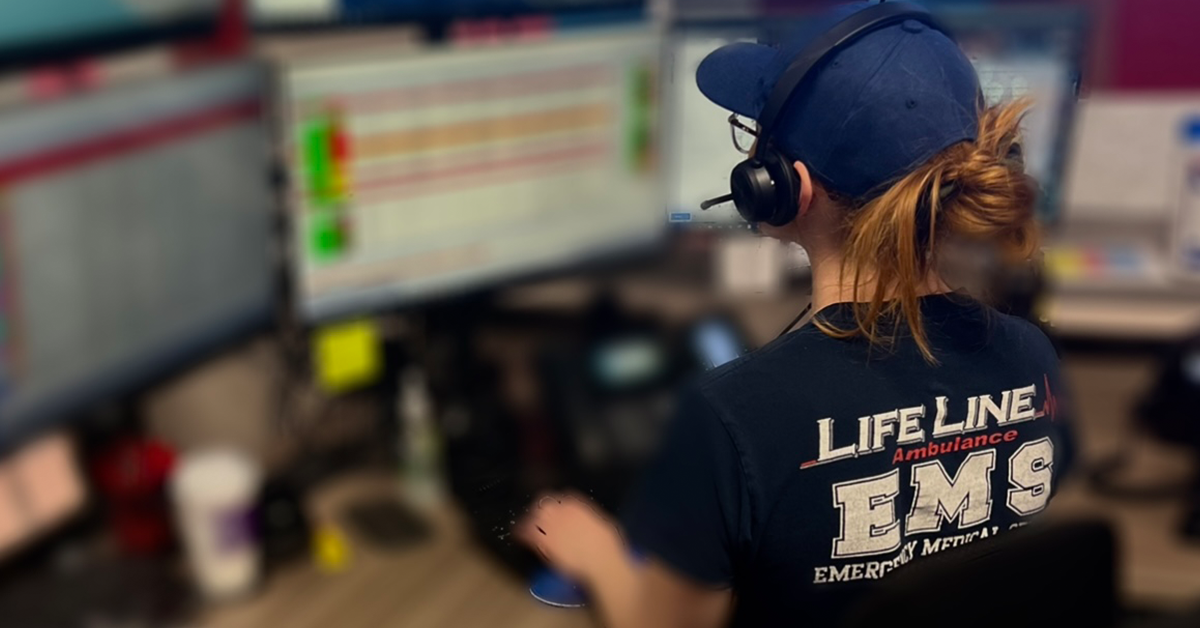
Step 1: Emergency Call and Dispatch Coordination
911 Call Initiation
- When an individual experiences a medical emergency, they dial 911.
- The call is received by a Public Safety Answering Point (PSAP), where trained dispatchers assess the situation.
Triage and Dispatch Assignment
- Dispatchers use standardized protocols to determine the severity of the emergency.
- Calls are categorized based on urgency, ranging from non-emergency medical transport to life-threatening conditions requiring immediate response.
- The dispatcher assigns the closest available LifeLine EMS unit, factoring in location, traffic conditions, and specialization needs (e.g., Advanced Life Support (ALS) vs. Basic Life Support (BLS)).
Step 2: EMS Unit Mobilization
Deployment and Navigation
- Once dispatched, the EMS team activates lights and sirens if necessary.
- Advanced GPS systems provide the fastest route to the patient, considering Los Angeles’ notorious traffic congestion.
- Some EMS teams utilize traffic preemption technology, which allows emergency vehicles to control traffic lights for expedited response.
Pre-Arrival Preparation
- En route, EMS personnel receive additional details from dispatch, including:
- Patient’s reported condition.
- Special considerations (e.g., hazardous environments, multiple patients).
- Required medical equipment (e.g., defibrillators for cardiac arrests).
- The crew mentally prepares for potential complications to ensure swift action upon arrival.
Step 3: On-Scene Patient Assessment and Treatment
Initial Scene Evaluation
- Upon arrival, EMS providers assess the safety of the environment before proceeding.
- First responders locate the patient and establish initial contact.
Primary Assessment
- Airway, Breathing, Circulation (ABCs): Immediate assessment to determine if the patient has life-threatening conditions.
- Vital Signs Monitoring: Heart rate, blood pressure, oxygen saturation, and other critical parameters.
- Patient History Collection: EMS personnel gather relevant information from the patient, family members, or bystanders.
Medical Interventions
- Depending on the severity of the case, EMS may perform:
- CPR and defibrillation for cardiac arrest patients.
- Oxygen administration for respiratory distress.
- Bleeding control using tourniquets or pressure bandages.
- Medication administration for allergic reactions, seizures, or diabetic emergencies.
- Splinting and immobilization for trauma victims.
Step 4: Transport Decision and Coordination
Determining the Destination
- The EMS crew decides whether the patient requires hospital transport or can be treated on-site.
- In critical cases, the nearest Level 1 Trauma Center or specialty hospital (e.g., stroke center, cardiac facility) is selected.
Pre-Arrival Hospital Notification
- EMS teams relay patient information to the receiving hospital to prepare medical staff for immediate intervention upon arrival.
- Paramedics provide an Electronic Patient Care Report (ePCR) detailing:
- Symptoms and initial assessment.
- Medical treatments provided.
- Response to interventions.
Safe Transport Execution
- The patient is secured in the ambulance with monitoring equipment.
- EMS personnel continue medical interventions during transit.
- Emergency driving techniques are used to balance speed with safety in high-traffic areas.
Step 5: Emergency Room Handoff
Arrival at the Hospital
- Upon reaching the hospital, EMS transfers the patient to medical staff.
- The team provides a verbal report summarizing:
- Patient’s condition upon arrival.
- Medical care provided en route.
- Response to treatment.
Post-Transport Documentation
- EMS personnel complete detailed documentation of the call for medical records and compliance purposes.
- If necessary, EMS teams debrief with hospital staff to discuss case complexities.
Step 6: Post-Call Procedures and Readiness for Next Call
Equipment Restocking and Sanitization
- Used medical supplies are replenished to ensure readiness for the next emergency.
- The ambulance interior is sanitized per strict infection control protocols.
Crew Debriefing and Mental Health Support
- For high-stress calls, EMS providers participate in critical incident debriefings.
- Mental health resources are available to address emotional stress from traumatic cases.
Returning to Service
- The EMS unit reports availability to dispatch and is reassigned based on regional needs.
Challenges in EMS Response and Solutions
Traffic Congestion in Los Angeles
- Solution: GPS tracking, traffic preemption systems, and optimized dispatching help mitigate delays.
Overloaded Emergency Rooms
- Solution: Triage protocols help prioritize transport to hospitals with available capacity.
Safety Risks for EMS Personnel
- Solution: Continuous training in defensive driving, self-defense, and handling hostile situations.
The Future of EMS Response in Southern California
EMS services are continuously evolving to improve efficiency and patient outcomes. Innovations include:
- Telemedicine Integration: Allowing paramedics to consult with ER doctors in real time.
- AI-Powered Predictive Analytics: Anticipating high-demand areas to deploy ambulances strategically.
- Drone-Assisted Emergency Response: Delivering medical supplies to remote locations faster.
- Wearable Health Monitoring Devices: Providing EMS teams with real-time patient data before arrival.
Keep Reading
Want more? Here are some other blog posts you might be interested in.
In the high-stakes world of emergency medical services, clear and effective communication can mean the difference between life and death. EMS professionals...
Emergency Medical Services is an ever-evolving field that requires constant learning and adaptation. With medical advancements, technological innovations, and increasing public health...
Emergency Medical Services s a high-stress, physically demanding profession that requires dedication, quick decision-making, and resilience. While the rewards of saving lives...